Pancreatic Cancer Symptoms
Endocrine: The endocrine glands secrete hormones, including insulin, into the bloodstream. Insulin also controls the levels of sugar in the blood.
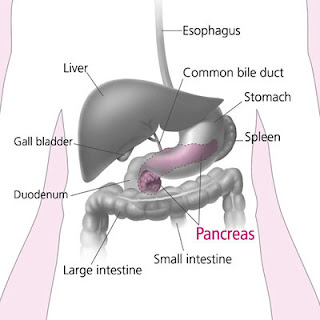
Head - The rightmost portion that lies adjacent to the duodenum
Uncinate process - An extension of the head of the pancreas
Body - The middle portion of the pancreas
Tail - The leftmost portion of the pancreas that lies adjacent to the spleen
Intraductal papillary mucinous neoplasia (IPMN) is a type of pancreatic cancer that is beginning to be recognized more frequently. This pancreatic cancer has a better prognosis than other types of pancreatic cancer. The most common type of pancreatic cancer arises from the exocrine glands and is called adenocarcinoma of the pancreas.
Pancreatic adenocarcinoma is among the most aggressive of all cancers. By the time that pancreatic cancer is diagnosed, most people already have disease that has spread to distant sites in the body. Pancreatic cancer is also relatively resistant to medical treatment, and the only potentially curative treatment is surgery. In 2004, approximately 31,800 people in the United States
This page has information on the symptoms of pancreatic cancer.
Symptoms from rare endocrine pancreatic tumours
Early symptoms
The commonest types of cancer of the pancreas
are exocrine tumours. Early symptoms can include
Weight loss
Pain in the stomach area
Jaundice
More early symptoms
Weight loss
People diagnosed with pancreatic cancer may have recently lost a lot of weight (at least 10% of their total body weight) for no apparent reason. This symptom is more common in cancers of the head of the pancreas.
Pain in the stomach area
About 7 out of 10 people with pancrea
tic cancer first go to their doctors because they have pain. Pain is more common in cancers of the body and tail of the pancreas.
Jaundice
Jaundice is yellowing of the skin and whites of the eyes. Jaundice is more common with cancer of the head of the pancreas because the tumour blocks the bile duct. This tube carries bile into the duodenum. Jaundice is a common symptom of many liver and gall bladder diseases.
More early symptoms
Other symptoms of pancreatic
cancer
There are other symptoms that you can have with cancer of the pancreas. Diabetes
Itching
Sickness
Bowel disturbances
Diabetes
Some people diagnosed with cancer of the pancreas are found to be newly diabetic. If you have diabetes you are not producing enough insulin. Weakness
Itching
You may have itching if you have bad jaundice. Sickness
You may feel or be sick because you have jaundice or an inflamed pan
creas. Bowel disturbances
Again, if you have jaundice you may develop a symptom called steatorrhoea. Symptoms from rare endocrine pancreatic tumours
There are rarer types of pancreatic cancer that produce hormones. These are the endocrine pancreatic tumours. The symptoms are different for each type, depending on the hormone the tumour produces.
Somatostatinomas produce too much of a hormone called somatostatin.